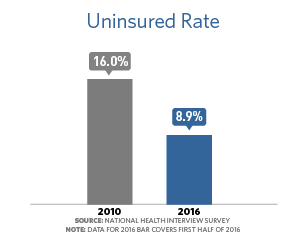
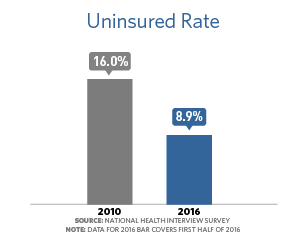
President Obama promised that he would make quality, affordable health care not a privilege, but a right. After nearly 100 years of talk, and decades of trying by presidents of both parties, that's exactly what he did. Today, 20 million more adults gained access to health coverage. We've driven the uninsured rate below 10 percent — the lowest level since we started keeping records — and built stronger, healthier communities through advancements in public health, science, and innovation.

Today, as many as 129 million Americans with pre-existing conditions can no longer be denied health coverage.
"Prohibited coverage denials and reduced benefits due to pre-existing conditions" → https://obamawhitehouse.archives.gov/the-record/health-care
HealthCare.gov: Ending Lifetime & Yearly Limits
"Insurance companies can’t set a dollar limit on what they spend on essential health benefits for your care during the entire time you’re enrolled in that plan."

2.3 million additional young adults (aged 19-25) gained health insurance coverage between the enactment of the Affordable Care Act in 2010 and the start of open enrollment in October 2013 due to the ACA provision allowing young adults to remain on a parent’s plan until age 26.
HealthCare.gov: Rescission
"Rescission is the retroactive cancellation of a health insurance policy. Insurance companies will sometimes retroactively cancel your entire policy if you made a mistake on your initial application when you buy an individual market insurance policy. Under the Affordable Care Act, rescission is illegal except in cases of fraud or intentional misrepresentation of material fact as prohibited by the terms of the plan or coverage."
Medicaid is Expanding Insurance Coverage
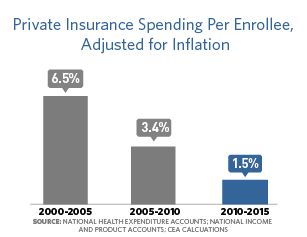
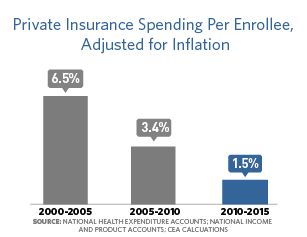
The U.S. has seen the sharpest reduction in the uninsured rate since the decade following the creation of Medicare and Medicaid in 1965, and the nation’s uninsured rate is now at its lowest level ever.
To learn more about the Health Insurance Marketplace, visit HealthCare.gov.
HealthCare.gov: How to Choose a Plan in the Health Insurance Marketplace
HealthCare.gov: How to Choose a Plan in the Health Insurance Marketplace → https://www.youtube.com/watch?v=XOkPAANg3R8
IRS: Individual Shared Responsibility Provision
HealthCare.gov: The Employer Shared Responsibility Payment
"Some employers with 50 or more FTE employees who don’t offer insurance, or whose offer of coverage is not affordable or doesn’t meet certain minimum standards, are subject to Employer Shared Responsibility provisions. They may owe a payment if at least one of their full-time employees enrolls in a plan through the Health Insurance Marketplace and receives a premium tax credit."
What Marketplace Health Insurance Plans Cover
Any plan shown in the Marketplace includes these essential health benefits. This is true for all plan categories (all “metal levels,” including Catastrophic plans) and all plan types (like HMO and PPO).
CMS: CHIP has provided meaningful health coverage to over eight million children.
"This program has helped cut the uninsured rate among children by nearly 60 percent since its start in 1997 – with more than one-quarter of that reduction since the President signed legislation reauthorizing the program in 2009."
Expanded Community Health Centers & incentives for primary care providers to practice in communities that need them: wh.gov/the-record/health-care
Created a new pathway to advance biosimilars, with the potential to lower costs for patients on high-cost biologics: wh.gov/the-record/health-care
Improving Access to Home- and Community-Based Services
In recent years, the Administration has expanded efforts to ensure that older adults and individuals with disabilities have access to person-centered services in community settings. For example, the Money Follows the Person Rebalancing demonstration helps states rebalance their Medicaid long-term services and supports systems and provides opportunities for older Americans and people with disabilities to transition back to the community from institutions. The Affordable Care Act extended and expanded this program.
Strengthening Health Care in Indian Country
Another critical step forward is implementing the Affordable Care Act, which contains many important benefits for American Indians and Alaska Natives. First and foremost, it includes the permanent reauthorization of the Indian Health Care Improvement Act, ensuring that the IHS is here to stay. It also improves benefits and protections for American Indians and Alaska Natives who have insurance, whether they receive care inside or outside the IHS. And it gives them more choices for health coverage, including Medicaid and the Federal Employees Health Benefits Program.
CMS: Early Retiree Reinsurance Program
"The Early Retiree Reinsurance Program (ERRP) was included in the Affordable Care Act (ACA) to provide financial assistance to employment-based health plan sponsors—including for-profit companies, schools and educational institutions, unions, State and local governments, religious organizations and other nonprofit plan sponsors—that make coverage available to millions of early retirees and their spouses, surviving spouses, and dependents."
Kaiser Family Health Foundation: Explaining the temporary high-risk pool
The health reform law created a temporary national high-risk pool to provide health coverage to people with pre-existing medical conditions who had been uninsured for six months. It was a temporary measure designed to bridge the gap until the implementation of other coverage provisions in the law that took effect in January 2014.
Created health plan disclosure requirements & summaries so consumers can evaluate coverage info & compare benefits: wh.gov/the-record/health-care
HHS: Maternal, Infant, and Early Childhood Home Visiting
"HRSA, in close partnership with the Administration for Children and Families (ACF), funds States, territories and tribal entities to develop and implement voluntary, evidence-based home visiting programs using models that are proven to improve child health and to be cost effective. These programs improve maternal and child health, prevent child abuse and neglect, encourage positive parenting, and promote child development and school readiness."
This Administration updated its comprehensive 2010 National HIV/AIDS Strategy for the United States through 2020, and implemented it alongside requirements to cover HIV screening for millions without additional cost and prohibit discrimination due to pre-existing conditions like HIV.
Read the Updated National HIV/AIDS Strategy:
What is a Health Center?
Health centers have played an essential role in the implementation of the Affordable Care Act and continue to be a critical element of the nation’s health system.
HHS Awards More Than $240 Million to Expand the Primary Care Workforce
The Affordable Care Act included funding for health provider training opportunities, with an emphasis on primary care, including a significant expansion of the National Health Service Corps. As of September 30, 2015, there were 9,600 Corps clinicians providing primary care services, compared to 3,600 clinicians in 2008.
Since 2008, more than 3 million additional children have gained health insurance.
Children have also seen important gains in insurance coverage in recent years, thanks in large part to improvements to CHIP signed into law by President Obama in 2009 and broader coverage expansions as a result of the ACA.
Read More: The Obama Administration issued a national strategy and a national action plan for domestic and international efforts to prevent, detect, and control illness and death related to infections caused by antibiotic-resistant bacteria.
Millions of Americans who are enrolled in Marketplace plans are receiving financial assistance to help them afford quality coverage.
Businesses with fewer than 25 employees may qualify for a tax credit worth up to 50 percent of their premium costs (up to 35 percent for tax exempt/non-profit employers).
Since September of 2013, the uninsured rate for women has dropped nearly 50 percent, meaning that about 9.5 million adult women have gained coverage.
Thanks to a provision in the Affordable Care Act, if your insurance company isn’t spending at least 80 percent of your premium dollars on medical care, they have to send you some money back.
The Affordable Care Act creates new incentives to promote workplace wellness programs and encourages employers to take more opportunities to support healthier workplaces. Effective for plan years after January 1, 2014, final rules allow the maximum reward to employers using a health-contingent wellness program to increase from 20 percent to 30 percent of the cost of health coverage, and the maximum reward for programs designed to prevent or reduce tobacco use will be as much as 50 percent.
Nearly 10.7 million Medicare beneficiaries have received discounts over $20.8 billion on prescription drugs – an average of $1,945 per beneficiary – since the enactment of the Affordable Care Act.
CMS Fact Sheet: Medicare Competitive Bidding Program Finds $42 Billion in Savings
"The overall savings to Medicare and beneficiaries as a result of the competitive bidding program for Durable Medical Equipment, Prosthetics, Orthotics, and Supplies is expected to total more than $42 billion over the first ten years of the program, according to the CMS Office of the Actuary. The $42 billion savings comes from a combination of savings of more than $25 billion in Medicare expenditures, and savings of over $17 billion for beneficiaries as a result of lower coinsurance payments and the downward effect on monthly premium payments."
The economic case for deploying new health care payment models:
Affordable Care Act Update: Implementing Medicare Cost Savings
Some cutting edge drugs are simply too expensive for many seniors. Creating a pathway for the approval of generic biologic drugs will improve affordability of medications for seniors and all Americans.
CMS: CMS expands quality data on Physician Compare and Hospital Compare to help consumers choose health care providers
“Consumers want trustworthy, reliable, and understandable information about the quality of health care delivered by providers,” said CMS Deputy Administrator and Chief Medical Officer Patrick Conway, M.D., MSc. “Both Physician Compare and Hospital Compare show consumers that they have a choice. This large release of quality measures for hospitals and physicians empowers consumers with information to make more informed health care decisions, encourages health care professionals to strive for higher levels of quality, and drives overall health system improvement.”
Patients Safer as Hospital-Acquired Conditions Decline
From 2010–2015, 21 percent of hospital-acquired conditions (HACs) such as adverse drug events, healthcare-associated infections, and pressure ulcers have been prevented in hospital patients. Reducing these HACs has saved an estimated 125,000 lives and nearly $28 billion in health care costs, according to HHS' annual report on patient safety.
The Administration set goals of tying 30 percent of traditional Medicare payments to alternative payment models by the end of 2016 and 50 percent by the end of 2018, and met its 2016 goal 11 months early.
Elder Justice Policy Brief
Elder abuse is a serious public health problem affecting millions of older Americans each year, with some studies suggesting that as few as one in 23 cases is reported to authorities. Elder abuse is defined as intentional actions that cause harm or create a serious risk of harm to an older person (whether or not harm is intended). Elder abuse encompasses physical abuse, neglect, financial exploitation, sexual abuse, as well as emotional and psychological abuse.
CMS Fraud Prevention Initiative
By using innovative predictive modeling technology similar to that used by credit card companies, CMS has stopped, prevented or identified $820 million in fraudulent payments over the past three years. The system identified or prevented $454 million in Calendar Year 2014 alone, a 10 to 1 return on investment.
IRS: New Requirements for 501(c)(3) Charitable Hospitals Under the Affordable Care Act
The Affordable Care Act added new requirements that hospitals must adhere to in order to qualify as a 501(c)(3) charitable hospital. The new requirements provide additional benefits to patients and their communities.
Questions and Answers for the Additional Medicare Tax
Why Open Payments is Important to You
Section 6002 of the Affordable Care Act requires the establishment of a transparency program, now known as Open payments. The program increases public awareness of financial relationships between drug and device manufacturers and certain health care providers.
The @WhiteHouse Record on Health Care: Required drug & medical-device manufacturers to publicly disclose info: wh.gov/the-record/health-care
The @WhiteHouse Record on Health Care: Required the posting of calorie information on menus of chain restaurants: wh.gov/the-record/health-care
Until the President made investments in health information technology by signing the American Recovery and Reinvestment Act, our health care system ran largely on paper. Now, more than 75 percent of doctors now use electronic health records thanks to Administration policies.
Learn more about electronic health records.
HHS.gov: HHS finalizes streamlined Medicare payment system that rewards clinicians for quality patient care
HHS finalized regulations to improve care and safety for nursing homes residents; Revisions mark first major rewrite of long-term care conditions of participation since 1991
The Centers for Medicare & Medicaid Services (CMS) issued a final rule to make major changes to improve the care and safety of the nearly 1.5 million residents in the more than 15,000 long-term care facilities that participate in the Medicare and Medicaid programs. The policies in this final rule are targeted at reducing unnecessary hospital readmissions and infections, improving the quality of care, and strengthening safety measures for residents in these facilities.
Remarks by the President and the Vice President at the 21st Century Cures Act Bill Signing
"Today, I could not be prouder that this legislation takes up the charge I laid out in my budget to provide $1 billion in funding so that Americans who want treatment can get started on the path to recovery and don’t have to drive six hours to do it. It is the right thing to do, and families are ready for the support."
SAMHSA to award nearly $1 billion in new grants to address the nation’s opioid crisis
Fact Sheet: Obama Administration Takes Action to Reduce Prescription Drug Shortages in the U.S.
The Administration finalized a regulation to expand access to opioid treatment by increasing the number of patient's physicians who can treat with the opioid use disorder treatment medication buprenorphine.
The change allows qualified physicians to prescribe buprenorphine to more patients. As of October 2016, 2,400 practitioners have applied for and been granted waivers to prescribe at the increased limit—improving access to buprenorphine, which is prescribed along with psychosocial supports as part of Medication-Assisted Treatment.
Read more about HHS’ change here.
The HHS also took action to enable nurse practitioners (NPs) and physician assistants (PAs) to begin taking the required training to prescribe the opioid use disorder treatment, buprenorphine.
Read more here.
The Administration also awarded $94 million in Affordable Care Act funding to 271 health centers across the country to increase substance use disorder treatment services, with a specific focus on expanding medication-assisted treatment of opioid use disorders in underserved communities.
See the map of communities here.
Read the CDC Guideline here.
Download the CDC checklist here.
The Administration also released an Opioid Overdose Prevention Toolkit for community members, first responders, prescribers, and patients and family members. The toolkit, developed by the Substance Abuse and Mental Health Services Administration, can be found here.
Fact Sheet: Obama Administration Announces Additional Actions to Address the Prescription Opioid Abuse and Heroin Epidemic
Additionally, the Administration awarded $1.8 million to rural communities to expand access to naloxone – a drug that reverses an opioid overdose and released Medicaid guidance to states identifying “Best Practices for Addressing Prescription Opioid Overdoses, Misuse and Addiction” including steps to increase the use of naloxone to reverse opioid overdose and to expand coverage of opioid use disorder treatment.
Read the Presidential Memorandum here:
Learn about the Health Insurance Marketplace:
HHS.gov: Administration issues final mental health and substance use disorder parity rule
The Administration also finalized a rule to implement parity protections in TRICARE, including expanding mental health and substance use disorder treatment to include coverage of intensive outpatient programs and treatment of opioid use disorders with medication-assisted treatment.
More than 893,000 pounds of unwanted medicines or about 447 tons were collected -- to help make homes safe from potential prescription drug abuse. Take-back days have collected and destroyed 5.5 million pounds of unused prescription drugs over five years.
Learn more about Tack-Back Day here:
The Administration also finalized a rule making it easier for communities to establish ongoing drug take-back programs to reduce the amount of unused prescription drugs in homes.
Read more about the US Drug Enforcement Administration’s final rule here.
White House Drug Policy Office Funds New Projects in High Intensity Drug Trafficking Areas
Read the Report here.
See the list of preventive services.
The Task Force met with parents, advocates, clinicians, health plans, regulators and others and developed a series of action steps and recommendations for future action to help ensure that mental health and substance use disorder benefits are treated at parity with medical and surgical benefits.
Learn more about the Clay Hunt Suicide Prevention for American Veterans (SAV) Act and the Administration's commitment to help veterans.
The White House hosts a National Conference on Mental Health at the White House as part of the Administration’s effort to launch a national conversation to increase understanding and awareness about mental health.
In response to the Executive Order, VA increased its mental health staffing, expanded the capacity of the Veterans Crisis Line, and enhanced its partnerships with community mental health providers; DoD and VA worked to increase suicide prevention awareness and, DoD, VA and the National Institutes of Health jointly developed the National Research Action Plan on military and veteran’s mental health to better coordinate federal research efforts.
The mental health executive actions fell under the following six categories:
FACT SHEET: President Obama Announces New Executive Actions to Fulfill our Promises to Service Members, Veterans, and Their Families
Vice President Biden Announces $100 Million to Increase Access to Mental Health Services
New investments in the Recovery Act, expanded through the Prevention and Public Health Fund in the Affordable Care Act, supported public-health initiatives that target heart disease, diabetes, and other conditions that afflict large segments of the population.
HHS: Prevention and Public Health Fund
The Affordable Care Act established the Prevention and Public Health Fund to provide expanded and sustained national investments in prevention and public health, to improve health outcomes, and to enhance health care quality. To date, the Fund has invested in a broad range of evidence-based activities including community and clinical prevention initiatives; research, surveillance and tracking; public health infrastructure; immunizations and screenings; tobacco prevention; and public health workforce and training.
FACT SHEET: The Family Smoking Prevention and Tobacco Control Act of 2009
FDA: Background on the FDA Food Safety Modernization Act (FSMA)
The FDA Food Safety Modernization Act (FSMA), signed into law by President Obama on Jan. 4, 2011, enables FDA to better protect public health by strengthening the food safety system. It enables FDA to focus more on preventing food safety problems rather than relying primarily on reacting to problems after they occur.
In 2009, First Lady Michelle Obama planted the White House Kitchen Garden on the South Lawn to initiate a national conversation around the health and wellbeing of the country. In time, that conversation led to Let's Move!. Through policy, programs, public awareness, and partnerships, Let’s Move! is about putting children on the path to a healthy future during their earliest months and years; giving parents helpful information and fostering environments that support healthy choices; providing healthier foods in our schools; ensuring that every family has access to healthy, affordable food; and helping children become more physically active.
The Healthy, Hunger-Free Kids Act updated school meal nutrition standards for the first time in 15 years and increased school meal funding for the first time in 30 years. The law boosted the quality and nutrition of meals for over 50 million children through the National School Lunch and Breakfast Programs. Its regulations substantially increased offerings of fruits, vegetables, and whole grains, and reduced the amount of saturated fat, trans fat and sodium.
Ensured that any food or beverage that is marketed on school campuses during the school day meets the Smart Snacks in School nutrition standards
Smart Snacks in School standards apply to foods sold a la carte, in the school store, and vending machines. This allows schools to offer healthier snack foods to children, while limiting junk food. Any food sold in schools must: Be a “whole grain-rich” grain product; or have as the first ingredient a fruit, a vegetable, a dairy product, or a protein food; or be a combination food that contains at least ¼ cup of fruit and/or vegetable; or contain 10% of the Daily Value of one of the nutrients of public health concern in the 2015 Dietary Guidelines for Americans (calcium, potassium, vitamin D, or dietary fiber).
Many of the foods and beverages that have been heavily marketed to children contribute to poor diet quality, high calorie intake, and excess weight gain. Foods offered and marketed to students during the school day now must be consistent with nutrition standards, so that any food or beverage that cannot be sold in school cannot be marketed in school either.
As part of the Healthy, Hunger-Free Kids Act, the Community Eligibility Provision impacts more than 18,000 schools in high poverty across the country that are eligible to serve free lunches and breakfasts to all students. It helps give 8.5 million American children access to free nutritious meals with no stigma and less time spent in cashier lines.
First Lady Michelle Obama announced the modernized Nutrition Facts label for packaged foods reflecting the latest science, the most relevant nutrition information and a refreshed design. Found on nearly 800,000 products, the label had not been significantly updated since its initial release twenty years ago.
In 2015, the Food and Drug Administration finalized its determination that partially hydrogenated oils (PHOs), the primary dietary source of artificial trans fat in processed foods, were no longer "generally recognized as safe” for use in human food. Food manufacturers are required to remove PHOs from products by 2018. This step is expected to reduce coronary heart disease and prevent thousands of fatal heart attacks every year.
Through the Healthy Lunchtime Challenge, First Lady Michelle Obama, in collaboration with the U.S. Departments of Agriculture and Education and a media partner, invited children ages 8-12, with the help of a parent or guardian, to create a lunch recipe that was original, healthy, affordable, and delicious. One winner from each U.S. state, territory, and the District of Columbia won the opportunity to attend the Kids’ “State Dinner” at the White House, where a selection of the winning recipes were served. Altogether, over 6,000 recipes were submitted and more than 270 young chefs and their families were welcomed to the White House for a total of five annual Kids’ “State Dinners.”
The Food and Drug Administration (FDA) Food Safety Modernization Act (FSMA), the most sweeping reform of our food safety laws in more than 70 years, was signed into law by President Obama on January 4, 2011. It enables FDA to better protect public health by strengthening the food safety system and to focus more on preventing food safety problems rather than relying primarily on reacting to problems after they occur.
The @WhiteHouse Record on Health Care: Required the posting of calorie information on menus of chain restaurants: wh.gov/the-record/health-care
For the first time in 20 years, the Department of Defense (DoD) updated their nutritional standards to include more fresh fruits, vegetables, whole grains, lean meats, and low-fat dairy products at the 1,100 service member dining facilities. Healthier foods were also made available at DoD schools and other areas where food is purchased on military bases, such as snack bars and vending machines.
The Agricultural Act of 2014 was enacted February 7, 2014. The law reauthorizes the Supplemental Nutrition Assistance Program (SNAP), the largest program in the domestic hunger safety net. It offers nutrition assistance to millions of eligible, low-income individuals and families and provides economic benefits to communities. The reauthorization of SNAP preserved the fundamental structure of the Program, and made a number of new investments such as providing $200 million for SNAP Employment and Training pilots to help participants find jobs and increase earnings, testing on-line grocery purchases, enhancing retailer standards, and helping participants stretch their dollars to purchase more fruits and vegetables.
Farmers’ markets and farm stands can now accept government benefits such as SNAP and coupons from participants in the Women, Infants and Children program from an electronic system.
During the school year, millions of children receive nutritious free and reduced price school meals through the USDA. However, less than a fifth of these children receive meals through USDA’s summer meals programs when school is out of session. As a result, low-income children are at higher risk of food insecurity and poor nutrition during the summer. The Summer EBT demonstration project is meant to help bridge that gap. It has showed a significant reduction in food insecurity among participating families and led to positive changes in children’s nutrition.
The Healthy Food Financing Initiative (HFFI) has brought grocery stores and other healthy food retailers to low-income, low-access communities in urban and rural communities across America. Without alternatives, residents of these communities often have to travel long distances to shop or rely on fast food restaurants and convenience stores that offer little or no fresh food. With technical assistance, improved access to capital, and financial support for retailers and other businesses in the food supply chain, HFFI is expanding access to nutritious food in these communities.
President Obama asked each member of his Cabinet to write an Exit Memo on the progress we’ve made, their vision for the country’s future, and the work that remains in order to achieve that vision. Here are their key points on the work ahead to improve health for all Americans.
Building on the Progress of the ACA
“Repealing the ACA, as some have suggested, risks rolling back consumer protections – like making it illegal to discriminate against those with pre-existing conditions and improving benefits – for Americans who get health insurance through the Marketplace, Medicare, Medicaid, or on the job. A recent study shows nearly 30 million Americans would lose their coverage under one version of repeal as well. We can work together to make the system even better, but we should build on the progress we’ve made, not go backwards.”
—Secretary Burwell
Reforming the Health Care Delivery System
“Building on the successful models developed during this Administration, while seeking out opportunities to extend value-based payment to an even broader range of providers and health care services, including high-cost drugs, not only benefits patients but allows clinicians the flexibility to practice medicine in the way that best meets the needs of their patients. The passage of MACRA was a monumental step forward in the effort to reward quality and value in physician payments; however, additional federal legislation should be considered that would use payment incentives to drive the delivery of value-based health care throughout the entire health care system, improve the interoperability of data, and integrate care.”
—Secretary Burwell
Developing Precision Medicine
“The next great revolution in medicine will emerge from an ability to use genomic, lifestyle, behavioral, environmental, imaging, and clinical data to understand health and disease, and to use those insights to develop tailored prevention approaches and medical treatments.”
—Director Holdren
Continuing the Fight against Opioids
“In late 2015, President Obama appointed me to lead an interagency federal effort focused on the rural heroin and prescription opioid crisis. In 2014 alone, we lost 28,648 lives too soon and according to NIH, the epidemic incurs $72 billion in health costs each year. The opioid crisis disproportionately affects rural communities in part due to the lack of outreach and treatment resources available in remote areas. After hearing from mothers and fathers who've lost their children to opioid misuse, and listening to mayors and medical personnel appeal for greater treatment resources, it's clear that rural communities need our help.”
—Secretary Vilsack
Combating the Global Threat of Infectious Diseases
“Continued high level U.S. leadership will be critical to maintain momentum and further institutionalize the gains that have been made, including through support to WHO and partners for external evaluations and country planning. U.S. leadership should include working with partners to follow through on their commitments, emphasizing the importance of country preparedness as a national priority, and highlighting the need for sectors beyond health, including the animal health, development, security, technology, and foreign affairs sectors, to support this work. Strengthening the multi-sectoral approach will benefit long-term health systems and the ability to respond effectively to outbreaks.”
—Secretary Burwell